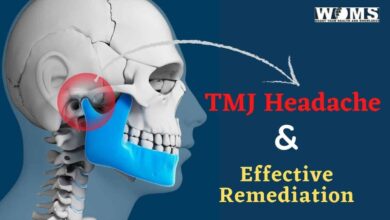
Is TMJ Jaw Pain Causing Your Headaches?

Temporomandibular joint disorder (TMJ) is a tricky disorder. This disorder in the joint near the ear creates a host of painful problems. Sadly, the temporomandibular joint is busy as you use it to talk and eat, so many people who have the disorder suffer from regular bouts of intense pain in the form of a TMJ headache.
Along with pain in the joint, many people with TMJ disorder experience headaches. Often, treating the headache gives temporary relief, but they usually return because the headache is a symptom and not the real problem. Fortunately, health care providers can treat TMJ headaches and help reduce the amount and pain of recurring headaches.
What Is TMJ and How Does It Cause a TMJ headache?
People have two temporomandibular joints near the ears, which connect your jaw to your skull. The joint allows the jaw to move up and down for common acts like talking and chewing. Like pain in other joints, the temporomandibular joint can have problems relating to
- Misalignment between the jaw and the skull
- Arthritis
- Trauma or injury
- Overuse
- Teeth grinding
- Tight muscles
Once problems arise in the temporomandibular joint, jaw pain often resembles headaches. About a third of the time, health care providers misdiagnose TMJ headaches as tension headaches because both types of headaches arise from muscle problems.
Your face has a fan-shaped muscle on either side of the face. Other important jaw muscles are near it in the cheeks. When these muscles tighten, they put pressure on the jaw joint and lead to a TMJ headache. Add that muscle tension to jaw misalignment, which puts more stress on the joint and eventually forces it out of alignment altogether.
Often, people with TMJ experience popping and clicking in the joint near the ear. This issue comes from the misalignment of the jaw and the disc between the jaw and the skull degenerating. The muscle pain from your misaligned jaw and temporomandibular joint causes pressure-related headaches.
How Do Healthcare Providers Diagnose TMJ?
When you report TMJ symptoms to your dentist, your dentist will follow steps to diagnose the problem. The dentist will check your jaw joints to feel for misalignment as well as grating or popping sounds and sensations. They will check your jaw’s range of motion to see how the problem limits your ability to bite. They will also check your facial muscles.
If your dentist suspects you have TMJ from the physical exam, your dentist will take X-rays or request an MRI or CT scan to see how much your jaw and the disc have degraded.
What Is The Standard Dental-Care Approach for this problem?
Treatment for TMJ headaches includes several standard approaches. As the problem is in the joint, dentists are usually the first line of care. Often, dentists first suggest making subtle lifestyle changes that help you relax and reduce tensing your jaw. Dentists also show their patients how to stretch to relax the muscles around the jaw. Some also suggest massage for more relief.
Dentists also suggest their patients record activities and foods that cause pain in the joint. They often suggest that their patients stop chewing gum and avoid other chewy foods and foods that require a wide-open jaw – like hamburgers and sandwiches.
Because patients with TMJ struggle to relax, their dentists recommend wearing an oral appliance that looks like an athletic mouthguard. Usually, dentists tell them to wear their mouthguard while sleeping to help them relax the jaw by preventing grinding and clenching. The appliance works to reposition your jaw if it is misaligned.
Occasionally, dentists use braces or invisible alignment devices if a mouthguard does not provide relief. As a last resort, dentists recommend oral surgery to repair the padding between the joints and remove excess fluid.
What Happens When Jaw Problems Go Untreated?
As TMJ comes from joint misalignment and degeneration, an untreated problem can worsen. The pressure from constant clenching and grinding can crack teeth and cause tooth loss. TMJ does not go away on its own.
Sometimes, people with TMJ struggle to sleep because they grind or clench while sleeping. Insomnia can cause depression and other psychological and health problems. People with TMJ often self-medicate to find relief, which can lead to alcohol or drug abuse.
Untreated TMJ also shows up in excessive tooth wear. People who have TMJ often favor one side when chewing, so muscle growth becomes asymmetrical, and some people experience facial swelling. If chewing becomes too painful, sufferers might stop eating healthy foods and turn only to soft foods and liquids, resulting in malnourishment.
TMJ can also cause ear pain, which can turn into tinnitus or hearing disorders. Inner ear problems can affect balance and dizziness, which can also affect your vision. It can also create serious jaw problems, where the jaw sticks open or closed. The disorder can also cause the jaw to become dislocated.
Why Wear Your Mouthguard?
If your dentist diagnoses TMJ, then you will most likely get a mouthguard or splint. Usually, your dentist will take an impression of your upper and lower teeth to make a customized splint that helps cushion your painful jaw.
Most patients with TMJ find relief with minor treatment, like wearing a mouthguard each night. If TMJ worsens, health care providers can recommend oral surgery, which can be risky due to the location of the pain and the extensive recovery period. Some surgeries do not work and worsen the condition.
Patients with TMJ can find relief while doing jaw exercises and stretches and by wearing a mouthguard as directed. Consistency matters when treating TMJ, so your splint needs to fit well and be comfortable.
Take Care of Jaw Pain Before It Worsens
TMJ can be extremely painful, causing headaches, muscle pain, and more problems. Some patients with TMJ find the pain so debilitating that they cannot go to work or go about their regular daily routine. Your health care providers can help you manage the pain with exercises, massage, and splints.