Dysfunctional uterine bleeding
Definition
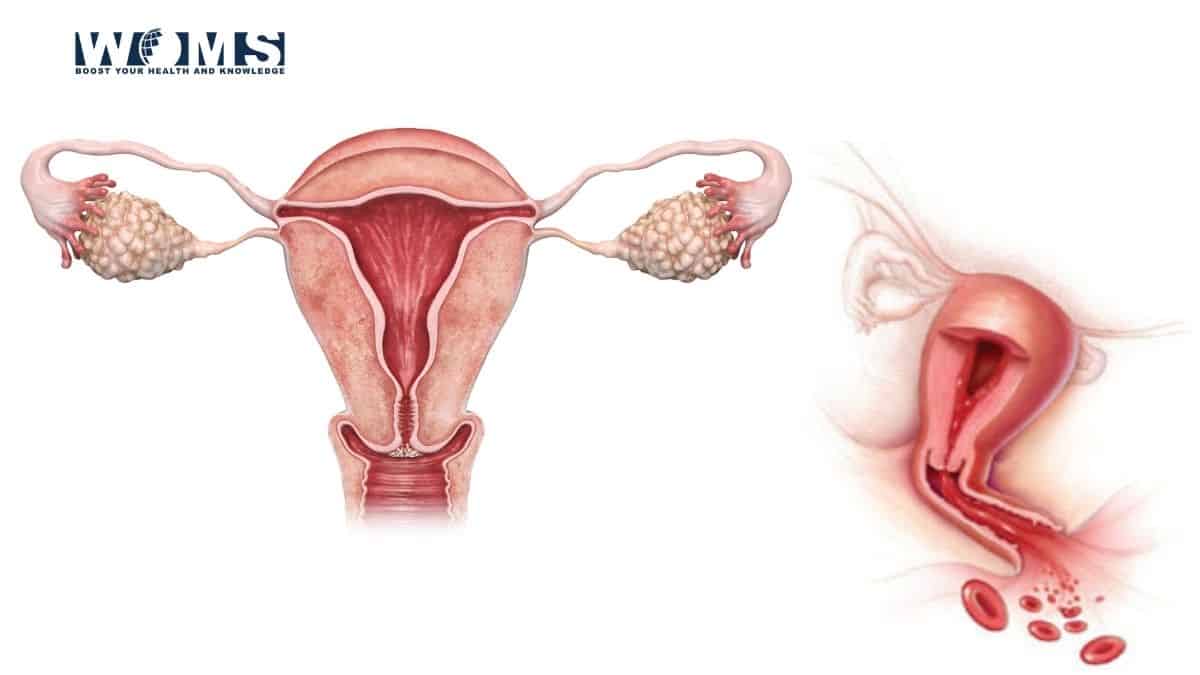
DUB: Dysfunctional uterine bleeding is defined as a frame of abnormal uterine bleeding without any clinically detectable organic, systemic and iatrogenic cause. [e.g. tumour, inflammation or pregnancy is excluded.
Key points
- Common causes of menorrhagia are Dysfunctional uterine bleeding, fibroid, adenomyosis or chronic pelvic infection.
- Common causes of contact bleeding are carcinoma cervix, cervical mucous polyp and vascular erosion.
- The endometrial pattern in dysfunctional uterine bleeding is secretory in 60 per cent and hyperplastic in about 30 per cent.
- In the late secretory phase, the level of both PGE2 and PGF2 in the endometrium increases and during menses PGF2a level rises over the PGE2. The menstrual blood loss is inversely related to the level of endometrial PGF2a/PGE2 ratio.
- In the acyclic type of bleeding, diagnostic D +C should be done within 24 hours of mates.
- DUB is a state of abnormal uterine bleeding due to anovulation predominantly.
- D +C misses the diagnosis of uterine lesions in 10-20 per cent of women as it is a blind procedure. D + C can stop the astute affair of excess uterine bleeding but not the subsequent episodes.
- Diagnostic tests in women with menorrhagia include measurement of haemoglobin, ferritin, TSH, endometrial biopsy and hysteroscopy.
- Hysteroscopy and biopsy are the best to evaluate the endometrial stature in DUB and to detect lesions such as submucous fibroid or polyp.
- To arrest acute episode of bleeding, potent progestogens are suitable in all periods of life, however, natural oestrogen administered parenterally (conjugated oestrogen 25 mg IV) is more effective in haemostasis during the early reproductive period.
- For cycle regulation, either progestogens or combined preparations of oestrogen and progestogen (pill) may be used.
- In refractory cases or in cases of temporary contraindication of surgery, danazol or GnRH analogues may be owned for short-term therapy.
- Prostaglandin synthetase inhibitors are effective in ovulatory DUB above the age of 35.
- Antifibrinolytic agents are suitable in case of DUB-following IUD.
- In cases of completed family, endometrial ablation/resection or hysterectomy is justified.
- Endometrial ablation or resection (TCRE) is done in a woman who is over 35 years, has completed her family and without any significant endometrial pathology (e.g. cancer, submucous fibroid > 10 cm in diameter).
- Ablation of endometrium up to a depth of 4-5 mm using laser, rollerball, thermal balloon, microwave, is an effective method. Resection of endometrium up to the basal layer is also a quicker and less costly method. Overall, amenorrhoea occurs in 50 per cent of women, about 40 per cent have decreased bleeding and 10 per cent may need a repeat procedure
hysterectomy - In the perimenopausal period, genital malignancy should be ruled out prior to any therapy.
Incidence
The prevalence varies widely but an incidence of 10 per cent amongst new patients attending the out-patient seems logical. The bleeding may be anomalistic in periodicity, amount or duration or combination of any three.
As the diagnosis is based on the exclusion of ‘organic lesion’, so with the care and facilities to exclude such a lesion, the incidence varies. Currently, many authors define Dysfunctional uterine bleeding as a state of abnormal uterine bleeding following anovulation due to dysfunction of the hypothalamic-pituitary-ovarian axis.
Pathophysiology
The current concept concludes that abnormal bleeding is most likely due to local causes in the endometrium. There is some disturbance of the endometrial blood vessels and capillaries and coagulation of blood in and around these vessels. These are probably related to alteration in the ratio of endometrial prostaglandins which are delicately balanced in haemostasis of menstruation.
The endometrial anomalism may be primary or secondary to incoordination in the hypothalamic-pituitary-ovarian axis. It is thus more prevalent in extremes of the reproductive period— adolescence and premenopause or following childbirth and abortion.
Heartwarming influences, worries, anxieties or sexual problems sometimes are enough to disturb the normal hormonal balance.
The abnormal anomalous may be associated with or without ovulation and accordingly grouped into :
- Ovular bleeding
- Anovulatory bleeding
Ovular bleeding
Polymenorrhoea or polymenorrhagia
The condition usually occurs following childbirth and abortion, during adolescence and premenopausal period and in pelvic inflammatory disease.
The follicular expansion is speeded up with resulting shortening of the follicular phase. This is probably due to hyperstimulation of the follicular growth by FSH. Almost never, the luteal phase may be shortened due to premature lysis of the corpus luteum. Sometimes, it is related to stress-induced stimulation.
Endometrial analyzing prior to or within a few hours of menstruation reveals secretory changes.
Oligomenorrhoea
Chief ovular oligomenorrhoea is rare. It may be met in adolescence and preceding menopause.
The disturbance may be due to ovarian unresponsiveness to FSH or secondary to pituitary dysfunction. There is an undue addendum of the proliferative phase with normal secretory phase.
Endometrial analyzing prior to or within a few hours of menstruation reveals secretory changes.
Functional menorrhagia
Ovular menorrhagia is quite freakish. Two arrays are found :
- capricious shedding of the endometrium.
- Irregular ripening of the endometrium.
Fluctuating shedding of the endometrium
The abnormality is usually met in extremes of the reproductive period.
Normally, regeneration of the endometrium is completed by the end of the third day of menstruation. In faltering shedding, desquamation is continued for a variable period with simultaneous failure of regeneration of the endometrium. The possible explanations are :
(i) Incomplete withdrawal of LH even on 26th day of cycle →9 incomplete atrophy of the corpus luteum →persistent secretion of progesterone.
(ii) Persistent LH →inhibition of FSH →9 suppresses ripening of the follicle in the next cycle→less oestrogen →less regeneration.
(iii) Variation of the endometrial receptors which are sensitive to the influence of oestrogen and progesterone.
Endometrial examine performed after 5th or 6th day of the onset of menstruation reveals a mixture of secretory and proliferative endometrium. There is a total absence of any surface epithelium.
Pregnanediol is found in the urine during the menstrual phase.
Eccentric ripening of the endometrium
There are poor formation and inadequate function of the corpus luteum. Secretion of both oestrogen and progesterone is inadequate to support endometrial growth. As like, slight bleeding occurs and continues prior to the start of proper flow.
The endocrine thumbnail in the luteal phase shows a persistent low level of urinary pregnanediol level of less than 3 mg or plasma progesterone akin less than 5 ng/ml.
Endometrial abstraction prior to or soon after spotting reveals a patchy area of secretory changes amidst proliferative endometrium.
Anovulatory bleeding
Menorrhagia
Anovulatory bleeding is usually excessive. In the truancy of growth-limiting progesterone due to anovulation, the endometrial growth is under the domination of oestrogen throughout the cycle. There is inadequate structural stromal support and the endometrium remains fragile.
As follows, with the withdrawal of oestrogen due to negative feedback action of FSH, the endometrial exfoliating continues for a longer period in asynchronous sequences because of lack of compactness.
This type of aberrant bleeding is usually met in premenopausal women.
The basic fault may lie in the ovaries or may be due to disturbance of the rhythmic secretion of the gonadotrophins. There is apatheticaccretion in the secretion of oestrogen but no negative feedback inhibition of FSH. The net effect is a gradual rise in the level of oestrogen with the concomitant phase of amenorrhoea for about 6-8 weeks.
As there is no ovulation, the endometrium is under the influence of oestrogen without being opposed by growth-limiting progesterone for a prolonged period. After a capricious period, however, the oestrogen level falls resulting in endometrial shedding with heavy bleeding.
Bleeding also betides when the endometrial growth have outgrown their blood supply. Due to increased endometrial thickness, tissue breakdown continues for a long time. Bleeding is heavy as there is no vasoconstrictor effect of PGF2(1. Bleeding is prolonged until the endometrium and blood vessels regenerate to control it.
Changes in the uterus
There is a variable degree of my hyperplasia with symmetrical enlargement of the uterus to a size of about 8-10 weeks due to simultaneous hypertrophy of muscles. The endometrial changes are Augustan. On naked eye examination, the endometrium looks thick, congested and often polypoidal (multiple Polyposis).
Microscopically
- There is marked hyperplasia of all the endometrial components. There is, however, intense cystic glandular hypertrophy rather than hyperplasia with the marked disparity in sizes. Few of the glands are small, others are largely giving the appearance of “Swiss cheese” arrangement (small and large holes of Swiss cheese made in Switzerland). The glands are empty and lined by columnar epithelium.
- Absence of secretory changes.
- Areas of necrosis in the superficial layers with small haemorrhages and leucocytic infiltration
Changes in the ovary
Cystic changes may be observed involving one or both the ovaries. The cyst may be single or multiple and the fluid contains oestrogen. The cyst is of follicular type. There is no evidence of corpus luteum.
Confusion in diagnosis
The phase of amenorrhoea followed by continued bleeding per vaginam with the bulky uterus is too oftentimes confused with disturbed uterine pregnancy or ectopic gestation. Dysfunctional uterine bleeding of this type is absolutely painless.
Atrophy of the endometrium
This type of abnormality is commonly met in postmenopausal women but they occur in reproductive aeon as a final evolutionary state of a previous metropathia.
The bleeding exposes from the rupture of the dilated capillaries beneath the atrophic surface epithelium. The cause of endometrial atrophy may be due to the total absence of oestrogen or failure of uterine receptors to become answering to oestrogen.
The endometrial pattern in Dysfunctional uterine bleeding
The following are the histological patterns found in Dysfunctional uterine bleeding. In the majority (60 the endometrium is normal secretory in every aspect. In about 30 per cent, the endometrium is hyperplastic and in the remaining, there are pieces of evidence of aimless shedding, irregular ripening or atrophic pattern.
Investigations
The investigation aims at :
- To confirm the menstrual abnormality as stated by the patient.
- To ban the ‘organic’ pelvic pathology.
- To identify the possible aetiology of Dysfunctional uterine bleeding.
- To work out the definite therapy protocol.
History
Firstly, it is to be confirmed that the bleeding is through the vagina and not from the urethra or rectum. The statement of excessive bleeding is assessed by the number of pads used, the passage of clots (size and number) and duration of bleeding. If ambiguity is found from the estimated haemoglobin percentage, it is better to appraise the blood loss by admitting the patient during the period. Among the patients presenting with menorrhagia, only about 50 per cent have got excess blood loss (> 80 ml).
Nature of menstrual abnormality is then to be enquired — cyclic or acyclic, its relation to adolescence, pregnancy events and last normal cycle. If there is a wrong interpretation of the cycle duration and there is no urgency of any therapy, it is better to explain her to keep the menstrual records for 2-3 cycles. Not only does it help in diagnosis but the spontaneous cure may occur on occasion.
Any excitable upset or psychosexual problem should be elicited tactfully. Use of steroidal contraceptives or IUCD insertion should be enquired. History of heteroclite bleeding from the injury site, epistaxis, gum bleeding or that suggestive of PID should be enquired.
A thorough general and relevant systemic examination are to be made in an effort to find out the cause or effect of abnormal bleeding. In a suspected case of thrombocytopenic purpura, tourniquet test is performed.
Internal examination
Bimanual grilling including speculum examination should be done in all cases except in celibate where the rectal examination is to be done to exclude palpable pelvic pathology. If the vaginal examination is required in virgins, it should be done under general anaesthesia and along with endometrial curettage.
Special investigations
- Blood values —- Haemoglobin estimation is done in every case. In pubertal menorrhagia not responding to usual therapy, platelet count, prothrombin time, bleeding time, fractional thromboplastin time are to be estimated. In suspected cases of thyroid dysfunction, serum TSH, T 3, T4 estimation is to be done.
- Diagnostic uterine curettage (D & C)
Indicative uterine curettage is indicated in Dysfunctional uterine bleeding —
(1) To exclude the organic lesions in the endometrium (incomplete abortion, endometrial polyp, tubercular endometritis or endometrial carcinoma).
(2) To arbitrate the functional state of the endometrium. (3) To have incidental therapeutic benefit.
In adolescent Dysfunctional uterine bleeding, it should be done if bleeding fails to stop or is severe in nature.
During the childbearing period (20-40 years), it should be done, if the bleeding is acyclic. Risk of endometrial carcinoma in this age group is very low. All the while premenopausal period, diagnostic curettage is mandatory prior to any therapy to exclude endometrial malignancy. During post Menopausal period, it is mandatory to exclude endometrial malignancy. Thin plastic endometrial sample (papillae) are available. It helps to obtain an adequate endometrial sample for histological examination. It is done as an OPD procedure without any anaesthetic.
- Ultrasound and colour Doppler findings of endometrial hyperplasia are: (i) Endometrial thickness>12mm. (ii)Hyperechoic and formal blueprint, (iii)Angiogenesis and neovascular signal study Transvaginal sonography (TVS) is also very sensitive to detect any anatomical abnormality (fibroid, adenomyosis) of the uterus, endometrium ( endometrial polyps) adnexa. Saline Infusion Sonography (SIS) is found very sensitive for the diagnosis of uterine pathology (polyps).
- Hysteroscopy– is done for better evaluation of endometrial lesion and take a biopsy from the offending site under direct vision. The frequent findings of polyps and submucous fibroid are often missed by blind curettage. Hysteroscopy and directed biopsy (H and B) can be performed as an out-patient basis. In many centres (H & B) has replaced conventional D and C
- Laparoscopy— to exclude unsuspected pelvic pathologies Such as endometriosis, PID or ovarian tumour (granulosa cell tumour). The indication is urgent if associated with pelvic pain.
- Hysterography — to exclude fibroid polyp or congenital malformation of uterus. Because Of reduced Specificity, HSG mostly replaced by hysteroscopy (Where facilities available).
Plan of special investigation.
Blood values →ultrasonography→ diagnostic uterine curettage/ endometrial sampling (papilla)→ hysteroscopy/hysterography→ laparoscopy.
Management
Because of diverse etiopathology of Dysfunctional uterine bleeding different phases of woman’s life, the management protocol has been grouped accordingly.
- Pubertal and adolescent menorrhagia< 20 years.
- Reproductive period (20-40 years)
- Premenopausal (>40 years)
- Postmenopausal
Reproductive Period
- General
- Medical
- Surgery
General
Rest is advised during the bleeding phase. Assurance and sympathetic handling are helpful particularly in adolescents. Anaemia should be corrected energetically by diet, haematinics and even by blood transfusion. Clinically evident systemic or endocrinal abnormalities should be investigated and treated accordingly.
Medical management of Dysfunctional uterine bleeding
Dysfunctional uterine bleeding (DUB), in the majority, responds well to conservative treatment during adolescence and early reproductive period. The derivatives of drugs used are listed in the table below.
Hormones: With the introduction of potent orally active progestins, they became the mainstay in the management of DUB in all age groups and practically replaced the isolated use of oestrogens and androgens.
Progesterone: The common preparations used are norethisterone acetate and medroxyprogesterone acetate. The latter one is better than the former as it does not alter the serum lipids. Mechanism of antiestrogenic action of progestins are: (i) It stimulates the enzyme (17-B-hydroxy steroid dehydrogenase) that converts oestradiol to oestrone (less potent). (ii) Inhibits induction of oestrogen receptor. (iii) It has an antimitotic effect on the endometrium. While confined progestins therapy is highly effective in an ovular dysfunctional uterine bleeding in ovular DUB combined preparations of progestogen and oestrogen (combined oral pills) are effective.
The foundation is used:
- Cyclic therapy Continuous therapy
To stop bleeding and regulate the cycle:
Norethisterone preparations (5 mg tab) are used thrice daily till bleeding clog which it usually does by 3-7 days.
| Medical management of dysfunctional uterine bleeding |
| (A)Hormones
· Norethisterone acetate · Medroxyprogesterone acetate · Dydrogesterone · Equine conjugated oestrogens · Combined oestrogens and progestogens (Contraceptive pills) · 19 Norsteroid derivative (Gestrinone) · Danazol (17 a-Ethinyl testosterone) · Progestine releasing IUCD LNG- IUS (p.459) · Mifepristone (RU 486) · GnRH analogues (p. 500) · Desmopressin |
| (B) prostaglandin synthetase inhibitors (PSI)
· Fenamates (Mefenamic acid) |
| (C) Antifibrinolytic agents
· Tranexamic acid (T A) · Ethamsylate · Epsilon aminocaproic acid (EACA) |
Cyclic therapy
- 5th to the 25th-day course.
- 15th to the 25th-day course.
5th to the 25th-day course:
In ovular bleeding — Any low prescription combined oral pills are cogent when given from 5th to 25th day of cycle for 3 continuing cycles. It causes endometrial atrophy. Normal menstruation is expected to resume with the restoration of normally functionating pituitary—ovarian-endometrial axis. It reduces menstrual blood loss by 50 per cent. It serves as a contraceptive as well.
In ovular bleeding — Cyclic progestogen preparation of medroxyprogesterone acetate 10 mg or norethisterone 5 mg is owned from 5th to 25th day of cycle for 3 cycles.
15th to the 25th-day course:
In ovular bleeding, where the patient famine pregnancy or in cases of aberrant shedding or aberrant ripening of the endometrium, dydrogesterone 1 tab (10 mg) daily or double a day from 15th to 25th day may aid the state. This regimen is, however, less effective than 5th to the 25th-day course. However, it does not suppress ovulation.
Continuous progestins: Synthetic progestins are widely used to treat menorrhagia. They counteract the effect of oestrogen, suppress the endometrium and the stroma is decidualised. Progestins also inhibit pituitary gonadotropin secretion and ovarian hormone production. Medroxyprogesterone acetate 10 mg thrice daily is inured and treatment is usually recapitulated for at least for 90 days.
Multitudinal continuous preparations may be used. Oral, long-acting intramuscular injections, implants, Progestogen-only bolus are effective to reduce menstrual blood loss. They may also conclude in oligomenorrhoea or amenorrhoea.
Oestrogen: In a locale where the bleeding is acute and severe, conjugated oestrogen 25 mg is given IV. It may be remade every four hours until the bleeding is controlled when oral therapy is started. Haemostasis is achieved by conjugated equine oestrogen 2.5 mg tablet given 4 times a day.
The bleeding usually stops within 2-3 days. In this situation, oestrogen stimulates regeneration of the denuded endometrium and controls bleeding by process of healing. The proliferation of the endometrium, increase in the level of fibrinogen, factors — V, X and platelet aggregation are the other mechanisms of action for oestrogen therapy. If bleeding recapitulates further, D and C are indicated.
Intrauterine progestogen— Levonorgestrel intrauterine system abet endometrial glandular atrophy, stromal decidualisation and endometrial cell inactivation. It is adequate for 5 years. It has basal systemic absorption. Reduction of blood loss is up to 97 per cent. Results are comparable to T CRE. It is considered as medical hysterectomy. In addition to its many other health benefits, it is an effective contraceptive measure.
Depot progestin preparations — have also been used to control excessive menstrual blood loss. Depot medroxyprogesterone acetate (DMPA) may cause amenorrhoea.
Danazol: Danazol is suitable in cases with recurrent symptoms and in patients waiting for hysterectomy. The dosages differ from 200-400 mg daily in 4 divided doses continuously for 3 months. A smaller dram tends to minimise the blood loss and a higher dose produces amenorrhoea.
Gestrinone: Gestrinone 2.5 mg orally twice a week for 3 months has been found useful. Mifepristone (RU 486): It is an anti-progesterone (19 nor steroid). It arrests ovulation and induces amenorrhoea and reduces myoma size.
GnRH agonists: The sub-therapeutic doses reduce the blood loss whereas in therapeutic doses produce amenorrhoea. It is valuable as short-term use in severe dysfunctional uterine bleeding, particularly if the woman is infertile and wants pregnancy. The drug is used subcutaneously or intranasally. It improves anaemia and is helpful when used before endometrial ablation (see below). A varying degree of hypo-oestrogenic features may appear.
Non-Hormonal management
Anti-fibrinolytic agents (Tranexamic acid) reduces menstrual blood loss by 50 per cent. It Counteracts the endometrial fibrinolytic system. It is decidedly conducive in IUCD induced menorrhagia. Gastrointestinal side effects are bourgeois. Antifibrinolytic agents can be used as first-line therapy.
Ethamsylate reduces endometrial capillary fragility. Results are often inconsistent.
Prostaglandin synthetase inhibitors: Mefenamic acid is much cogent in women aged more than 35 years and in cases of ovulatory dysfunctional uterine bleeding. The dosage of medicine is 150-600 mg orally in divided doses during the bleeding phase.
The Fenamates inhibit the synthesis of prostaglandins and interfere with the binding of PGE2 to its receptor. NSAIDs can reduce menstrual blood loss by 25-40 per cent. Improvement of dysmenorrhoea headache or nausea are the added benefits. Side effects are often balmy. NSAIDs may be used as first-line medical treatment.
Desmopressin — is a synthetic analogue of arginine —vasopressin. It is specially indicated in cases with von Willebrand’s disease and factor VIII deficiency. It is given IV (0.3 gs/kg) or intranasally.
Surgical management of Dysfunctional uterine bleeding
- Uterine curettage
- Endometrial abscission.
Uterine curettage
It is done predominantly as a diagnostic tool but at times, it has got the haemostatic and therapeutic effect by abolishing the necrosed and unhealthy endometrium. It is hopefully expected that the normal relation of the hypothalamic-pituitary-ovarian-endometrial axis is re-established by the time the regeneration of the endometrium occurs. The adumbration is a chief one, if the bleeding is acyclic and where endometrial pathology is suspected.
Endometrial ablation/resection
Indications are:(i) Women who have failed to respond medical treatment (ii) Where hysterectomy is risky or the patient is unfit for longer duration surgery or because of obesity or adhesion (iii) When the patient prefers to preserve her uterus.
- Laser ablation of the endometrium using the Nd: YAG laser through hysteroscope is an alternative to hysterectomy. It is employed as an elective alternative to hysterectomy or when hysterectomy has been medically contraindicated. Tissue destruction (coagulation, vaporisation and carbonisation) to a depth of 4-5 mm produces a therapeutic Asherman’s syndrome and The method should be employed in cases who have completed their families.
- Transcervical resection of the endometrium (TCRE) through continuous flow resectoscope is quicker and less costly than laser ablation. It can be borne out even under the paracervical block. Resectoscope loop must abolish the basal layer of endometrium along with the superficial layer of myometrium otherwise metamorphosis of endometrium causes the failure of the operation.
- Rollerball ablation of the endometrium is also effective. It coagulates endometrium up to a depth of about 4 mm.
Complications
Uterine perforations, fluid absorption may occur during the hysteroscopic procedure.
- Uterine thermal balloon for the destruction of the endometrium is currently used with a satisfactory result. The endometrium is destroyed using a thermal balloon with hot normal saline (850C) for 10-15 minutes. No dilatation of the cervical canal is needed. This procedure is suitable for are not suitable for general anaesthetic or long-duration surgery. The success rate is similar to TCRE. No pretreatment GnRH analogue is required. This is commonly done as a daycare basis.
- Microwave endometrial ablation is carried out as an out-patient procedure. Microwave electromagnetic heat energy causes ablation of the endometrium. Endometrial tissue up to a depth of 6mm is ablated. The temperature in the region in 75-800 Treat time (2-3 minutes) is less compared to TCRE.
- Novasure: Endometrial ablation is done a bipolar electrode array mounted on an expandable frame. This creates a confluent lesion on the entire endometrial surface. The time required for global endometrial ablation is 90 seconds approximately-Radio frequency energy vaporises or coagulates the endometrium up to the myometrium. Women with uterine cavity < 4 cm, PID, caesarean delivery are contraindicated.
Pretreatment with danazol or GnRH agonists to make the endometrium atrophic. The limitations and effectiveness of endometrial ablation should be carefully evaluated before its wider application.
Results of Endometrial Ablation or Resection
Overall success with these methods is 70-80 per cent. About 40-50 per cent of women become amenorrhoeic and another 40 per cent will have significant improvement in heavy blood loss. But 10 per cent of women may need to repeat procedure or hysterectomy. For case druthers, side effects, contraindications and complication.
Hysterectomy
Hysterectomy is justified when the conservative treatment fails and the blood loss impairs the health of the patient. Presence of endometrial hyperplasia and atypia on endometrial histology is an indication for hysterectomy. The decision can be taken easily as the patient is approaching 40.
But even in women of thirties, prolonged procrastination with the persistence of symptoms in spite of hormone therapy is often an indication of hysterectomy specially in those having a desirable number of children. Ovaries, however, are to be preserved. The alternative in this group is endometrial ablation.




