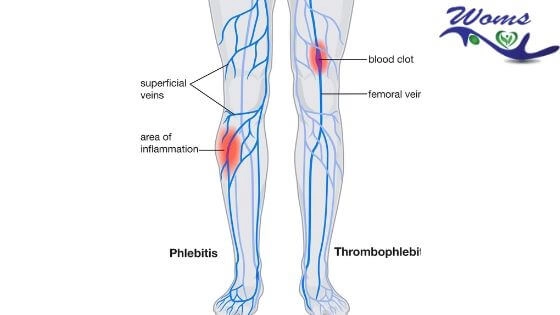
Phlebitis and Thrombophlebitis
What should you know about phlebitis and thrombophlebitis?
Phlebitis is outlining as the inflammation of the vein. It can be caused by any insult to the blood vessel wall, impaired venous flow, or coagulation abnormality.
Thrombophlebitis is also defined as the inflammation of the vein due to the formation of a blood clot associated with phlebitis. It can be superficial thrombophlebitis or deep thrombophlebitis.
What is phlebitis?
The lower limb is the most common site of venous disorders. More than 5% of the population have varicose veins, and 1% have, or have had, venous ulceration. At any one time, up to 200 000 people in the UK have active venous ulceration.
(Fle-BYE-tis) is inflammation vein due to many causes like extended periods of inactivity or immobility, varicose veins, and many more. It can be painful but not life-threatening. People with phlebitis have a 20 to 40 percent chance of also having DVT.
What is Thrombophlebitis?
It is the inflammation of veins, usually of superficial veins due to different causes. It is a superficial vein thrombosis (SVT) with inflammation (sight).
Types of phlebitis
Phlebitis can be of two types, i.e, superficial, and deep.
Let us now know what does superficial means. Superficial phlebitis outlined as the inflammation of a vein near the surface of your skin. Superficial phlebitis may require treatment, but isn’t usually critical. It can result from a blood clot or other causes like irritation from an intravenous catheter.
Deep phlebitis outlined as inflammation of a more in-depth, larger vein, which is mainly found in your legs. It is more likely to caused by a blood clot, which has serious, life-threatening consequences. It’s essential to know the risk factors and symptoms of a DVT.
Types of thrombophlebitis
- Acute: due to IV cannulation, trauma, minor infections, hypercoagulability.
- Recurrent
- Spontaneous: polycythemia vera, polyarteritis, burger’s disease.
- Thrombophlebitis migrans (trousseaus; sign): spontaneous migrating thrombophlebitis seen in visceral malignancy like pancreas, stomach.
- Mondor’s disease
Symptoms of phlebitis
It can be seen either in the upper limb or lower limb. These symptoms include:
- Pain
- Redness
- Tenderness
- Cord like thickening of veins
- Fever
Phlebitis causes
It has many causes. Some of the common causes of phlebitis are:
- Superficial phlebitis can be an aggravation due to a medical or surgical procedure.
- Local trauma or injury to the vein
- Prolonged inactivity or immobility: such as staying in bed or sitting for many hours, as in a car or an airplane, long motor rides, etc.
- Sedentary lifestyle
- Obesity
- Cigarettes smoking
- Insertion of intravenous catheter induced it.
- Postoperative period especially after orthopedics surgery
- Sustained immobility, as in hospitalized or bed-ridden patients
- Varicose vein
- Certain blood disorders, or underlying cancers or clotting disorders
- Trauma to arm or leg
- Pregnancy
- Hormone replacement therapy or birth control pills
- Infections
- Intravenous drug use
- Burn patients
Who is at risk?
One of the common risk factors for phlebitis is trauma. So people with injury mainly in legs and arm are at risk of it.
- The person with a history of DVT
- Blood clotting disorders, such as factor V Leiden
- Hormone therapy or contraceptive pills
- Prolix immobility is another common risk factor for phlebitis
- Sitting for long periods, such as during travel
- Underlying cancers and cancer treatments
- Pregnancy
- Obesity
- People having a sedentary lifestyle
- History of recent surgery mainly orthopedics surgery
- Smoking
- Alcohol abuse
- Age over 60
What are the complications of phlebitis?
- Destruction of venous valves resulting in varicose vein
- DVT
- Embolism
- Infection
Phlebitis treatment
- Elevation
- Anti-inflammatory drugs, antibiotics
- Application of crepe bandage-compression therapy
- Anticoagulation-LMWH for SVT> 3cm in length
Heparin should not be given intramuscularly and should not be combined with streptokinase or urokinase. Heparin is not given orally. Heparin administration should be monitored with APIT.
Prevention to phlebitis
Many people write Flebitis instead of phlebitis. Indeed, sometimes we can’t avoid it, but still, we can take proper prevention of it. According to specialists in varicose veins Scottsdale, we can apply some simple measures to prevent it. Some of the preventive measures of phlebitis and thrombophlebitis are as follows:
- After any surgery or such treatments, there should be early management
- If you are going on a long journey or ride, you should regularly perform leg exercises
- Smoking should be avoided
- Maintenance of good nursing hygiene should be done
Mostly in deep venous phlebitis, afterwards, there may be a requirement of compression stockings—measures like this help to reduce the chances of recurrent phlebitis. Moreover, applying appropriate measures also help to mitigate post-phlebitic swellings.
There are also cases of hospitalized phlebitis patients having low mobility available. In that case, a small dose of blood thinners may be given. This helps to avoid the formation of a blood clot by keeping the blood relatively thin. This type of prescription that is provided for prevention is relatively low that those given for the treatment of existing blood clots.
Is walking good for phlebitis?
You may be wondering that in phlebitis, bed rest might be mandatory as in most injuries. But this is not the case. Regular exercise, mainly walking, is suitable for phlebitis. Walking or exercising helps to improve blood flow. So keep walking to prevent it and make sure you avoid injecting illegal drugs to your veins in the name of treatment. Also, prevent yourself from infections and all.
we hope you have good knowledge of phlebitis and thrombophlebitis.