Infective Endocarditis
Etiology I Risk factors I Clinical features I Pathogenesis I Investigations I Complications I Treatment
What is Infective Endocarditis?
Infective endocarditis is an inflammatory disorder, mainly of the cardiac valves, that results from infection by any of several types of microorganisms, including bacteria, fungi, rickettsiae, and viruses.
Acute endocarditis is an agitatedly fevered illness that briskly blemishes cardiac structures, and hematogenous seeds in extracardiac sites, and if untreated, progresses to death within weeks.
Aetiology
- Streptococcus viridans: More common after a dental procedure.
- Staphylococcus aureus and Staphylococcus Epidermidis: Common inpatient with no underlying heart diseases.
- Enterococcus: Common after lower bowel or genitourinary manipulation.
- Pseudomonas aeruginosa: More common in intravenous drug abusers.
- Culture negative (10% of cases).
Risk Factors
- Children with acquired valvular disease
- Children with congenital heart disease
- Intravenous drug abuse
- Children with central venous line
- Poor oral hygiene
- No antibiotic coverage during minor or major surgical intervention
Pathogenesis
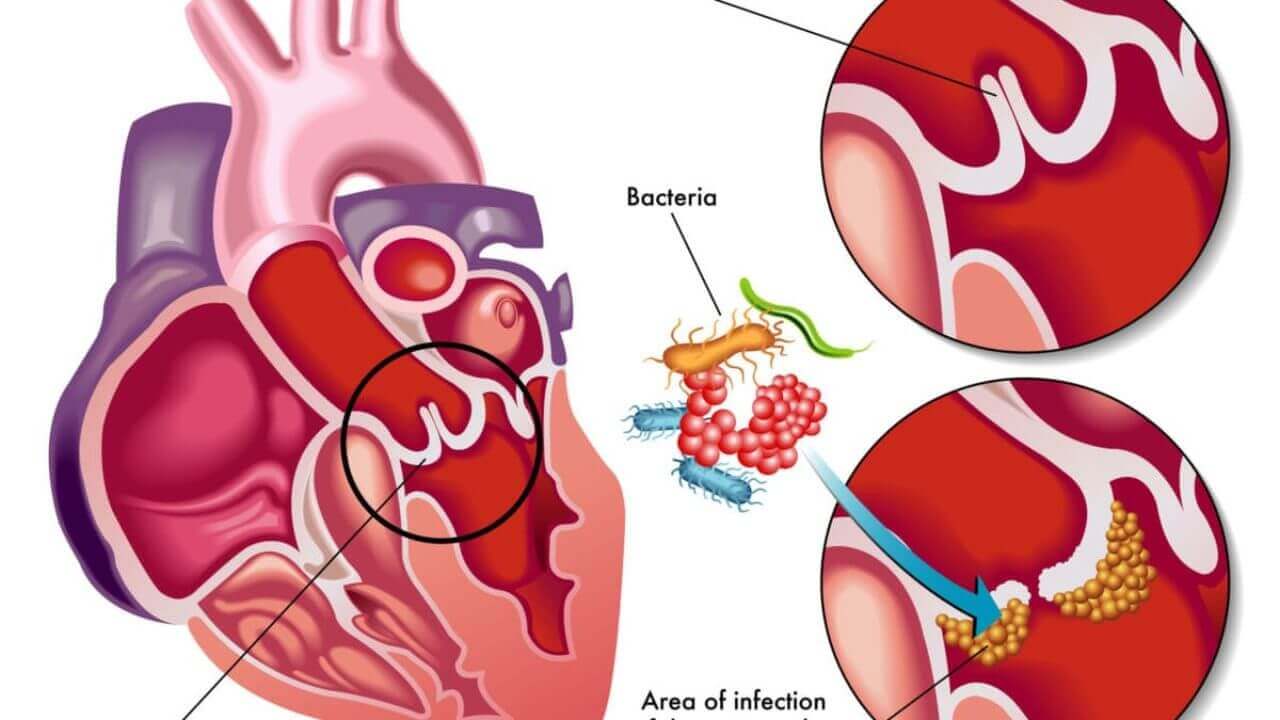
Endocarditis develops when a jet of blood, turbulence, or trauma leads to cardiac endothelial damage, which serves as the nidus for bacterial infection. In most cases, oral bacteria, which intermittently invade the bloodstream, infect the damaged endothelium.
The prototypic lesion at the site of infection, the ‘vegetation’, is a mass of platelets, fibrin, microcolonies of microorganisms and scanty inflammatory cells. They may be single or multiple and range in size from a few millimetres to several centimetres. Pieces of the vegetations may break off and cause embolization (e.g., Roth’s spot, splinter haemorrhage).
Clinical Features
- Symptoms of infective endocarditis: Fever, chills, night sweats, myalgia, arthralgia, loin pain, neurological manifestation (stroke, seizure, headache), dyspnea.
- Signs of infective endocarditis: Tachycardia, clubbing, hematuria, new or worsening regurgitant murmur, splenomegaly, petechial rash, peripheral manifestation due to embolism (Osler node, splinter haemorrhage in the nail bed, Janeway lesion, Roth spot), arrhythmia, heart failure.
Complications
- Cardiac: Valvular insufficiency or stenosis with cardiac failure, myocardial ring abscess, suppurative pericarditis
- Embolic: Left-sided lesion—brain (cerebral abscess, meningitis), spleen (abscess), kidney (abscess). Right-sided lesion——lungs (abscess,pneumonia)
- Renal: Infarction, focal glomerulonephritis leading to nephrotic syndrome or renal failure, diffuse glomerulonephritis leading to renal failure
- Depression may occur due to prolonged hospitalization.
Cardiovascular disease
Organisms Causing Endocarditis, Choice of Antibiotics, and Duration of Treatment
| Organism | Option I | Option II | Duration |
| Streptococcus
viridans | Penicillin and
aminoglycoside | Cefazolin and
aminoglycoside | 4 wk |
| Group A
streptococci | Penicillin and
aminoglycoside | Cefazolin and
aminoglycoside | 4 wk |
| Streptococcus
Faecalis | Ampicillin and
aminoglycoside | Vancomycin and
aminoglycoside | 6 wk |
| Staphylococcus
aureus | Cloxacillin and
aminoglycoside | Vancomycin and
aminoglycoside | 6 wk |
| Escherichia coli | Ceftriaxone and
aminoglycoside | Ampicillin and
aminoglycoside | 6 wk |
| Pseudomonas | Ticarcillin and
aminoglycoside | 6 wk | |
| Culture negative | Ampicillin and
aminoglycoside | Cloxacillin and
aminoglycoside | 6 wk |
Principles of management
Principles of management are
- (i) identification of the organism;
- (ii) determining its antibiotic sensitivity; (
- iii) starting treatment as early as possible; and
- (iv) using a bactericidal antimicrobial agent(s) for an appropriate duration to obtain a cure and prevent relapse.
If the blood culture is positive, the choice of antibiotics is dictated by the antibiotic sensitivity. If the culture is negative, empirical therapy covering a wide range of organisms is necessary. Organisms causing endocarditis, choice of antibiotics, and duration of treatment depict the prophylactic measures to be taken during dental procedures and genitourinary and gastrointestinal operations.
Note: High serum bactericidal levels must be maintained long enough to eradicate organisms that are growing in relatively inaccessible avascular vegetations.
From 5 to 20 times the minimum in vitro inhibiting concentration must be produced at the site of infection to destroy bacteria growing at the core of these lesions. Several weeks are required for vegetation to organize completely thus therapy must be continued through this period, so that recrudescence can be avoided. A total of 4-6 weeks of treatment is recommended.
Complications
- Cardiac: Valvular insufficiency or stenosis with cardiac failure, myocardial ring abscess, suppurative pericarditis.
- Embolic: Left-sided lesion—brain (cerebral abscess, meningitis), spleen (abscess), kidney (abscess). Right-sided lesion—lungs (abscess, pneumonia)
- Renal: Infarction, focal glomerulonephritis leading to nephrotic syndrome or renal failure, diffuse glomerulonephritis leading to renal failure.
- Depression may occur due to prolonged hospitalization.
Investigations
- Blood culture: At least three blood cultures within 24 hours from three different venepunctures, with at least I hour gap between two punctures (Positive > 90% cases).
- Leukocytosis, low haemoglobin content, proteinuria, microscopic hematuria, raised ESR and CRP, hypergammaglobulinemia, hypocomplementemia, rheumatoid factor (+ve), high blood urea, and serum creatinine levels.
- ECG may reveal conduction defect due to abscess formation pr infarction due to emboli.
- Chest x-ray shows evidence of cardiomegaly or heart failure.
- Echocardiography for detection of valve vegetations.
Infective Endocarditis Treatment
The treatment of endocarditis can be considered under the two headings—
- Treatment of the current episode and
- prevention of endocarditis.
General FAQs
How serious is infective endocarditis?
Mitral valve vegetation caused by bacterial endocarditis. Infective endocarditis is an infection of the inner appearance of the heart, usually the valves. Evidence may include fever, small areas of bleeding into the skin, heart murmur, feeling tired, and low red blood cell count.
What causes petechiae in infective endocarditis?
Conjunctival petechiae, Osler’s, and splinter haemorrhages represent vascular phenomena caused by endovascular infection, most commonly acute infective endocarditis. These findings can also rarely be seen in other endovascular infections such as aortic graft infections




