Adenocarcinoma of the pancreas
Some 90% of pancreatic neoplasms are adenocarcinomas that arise from pancreatic ducts. These tumours involve local structures and metastasise to regional lymph nodes at an early stage. Most patients have advanced disease at the time of presentation. Neuroendocrine tumours also arise in the pancreas but tend to grow more slowly and have a better prognosis. Pancreatic adenocarcinoma affects 10-15 per 100 000 in western populations, rising to 100 per 100 000 in those over the age of 70. Men are affected twice as often as women.
The disease is associated with increasing age, smoking and chronic pancreatitis. Between 5% and 10% of patients have a genetic predisposition: hereditary pancreatitis, HNPCC and familial atypical mole multiple melanoma syndrome (GAMMM). Overall survival is only 3-5%, with a median survival of 6-10 months for those with locally advanced disease and 30-5 months if metastases are present.
Clinical features
Many patients are asymptomatic until an advanced stage when they present with central abdominal pain, weight loss and obstructive jaundice. The pain results from the invasion of the coeliac plexus and is characteristically incessant and gnawing. It often radiates from the upper abdomen through to the back and maybe eased a little by bending forwards. Almost all patients lose weight and many are cachectic.
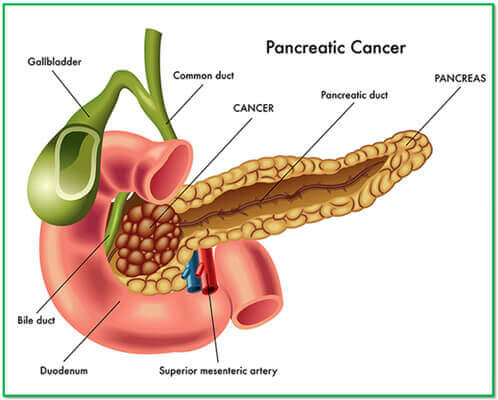
Around 60% of tumours arise from the head of the pancreas, and involvement of the common bile duct results in the development of obstructive jaundice, often with severe pruritus. A few patients present with diarrhoea, vomiting from duodenal obstruction, diabetes mellitus, recurrent venous thrombosis, acute pancreatitis or depression. Physical examination reveals clear evidence of weight loss. An abdominal mass due to the tumour itself, a palpable gallbladder in a jaundiced patient is usually the consequence of distal biliary obstruction by pancreatic cancer (Courvoisier’s sign).
Investigations
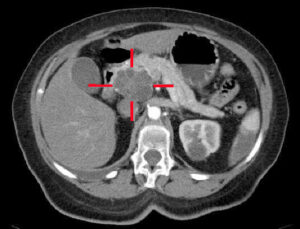
The diagnosis is usually made by ultrasound and contrast-enhanced CT. Diagnosis in non-jaundiced patients is often delayed because presenting symptoms are relatively non-specific. Fit patients with small, localised tumours should undergo staging to define operability. EUS or laparoscopy with laparoscopic ultrasound will define tumour size, the involvement of blood vessels and metastatic spread.
In patients unsuitable for surgery because of advanced disease, frailty or comorbidity, EUS-or CT guided cytology or biopsy can be used to confirm the diagnosis. MRCP and ERCP are sensitive methods of diagnosing pancreatic cancer and are valuable when the diagnosis is in doubt, although differentiation between cancer and localized chronic pancreatitis can be difficult. The main role of ERCP is to insert a stent into the common bile duct to relieve obstructive jaundice in inoperable patients.
Management
Surgical resection is the only method of effecting the cure, and 5-year survival in patients undergo a complete resection is around 12%. Clinical trials have demonstrated improved survival (21-29%) with adjuvant chemotherapy using gemcitabine. Unfortunately, only 10-15% of tumours are resectable for a cure, since most are locally advanced at the time of diagnosis. For the great majority of the patients, treatment is palliative.
Chemotherapy with FOLFIRINOX (5-fluorouracil, leucovorin, irinotecan and oxaliplatin) improves median survival to 11 months. Pain relief can be achieved by using analgesic but, in some patients, coeliac plexus neurolysis may be required. Jaundice can be relieved by choledochojejunostomy in fit patients, whereas percutaneous or endoscopic stenting is preferable in the elderly and those with very advanced disease. Ampullary or periampullary adenocarcinomas are rare neoplasms that arise from the ampulla of Vater or adjacent duodenum.
They are often polypoid and may ulcerate; they frequently infiltrate the duodenum but behaves less aggressively than pancreatic adenocarcinoma. Around 25% of patients undergoing resection of periampullary tumours survive for 5 years, in contrast to patients with pancreatic ductal cancer.
Incidental pancreatic mass
Cystic neoplasms of the pancreas are increasingly being seen with the widespread use of CT. These are heterogeneous group; serous cystadenomas rarely, if ever, become malignant and don’t require surgery. Mucinous cysts occur more often in women, are usually in the pancreatic tail and display a spectrum of behaviour fro benign to frankly malignant.
Aspiration of the cyst contents for cytology and measurement of CEA and amylase concentrations in fluid obtained at EUS can help determine whether a lesion is mucinous or not. IN fit patients, all mucinous lesions should be resected. A variant, called intraductal papillary mucinous neoplasia (IPMN), is often discovered coincidentally on CT, frequently in elderly men. This may affect the main pancreatic duct with marked dilatation and plugs of mucus or may involve a side branch.
The histology varies from villous adenocarcenatous change to dysplasia or carcinoma. Since IPMN is a pre-malignant but indolent condition, the decisions to reset or to monitor depends on age and fitness of the patients and location, size and evolution of lesions.