Myasthenia Gravis Symptoms [Investigations & Treatment]

Myasthenia Gravis is defined as the neuromuscular disorder that causes weakness in the skeletal muscles, which skeletal muscles is used as the movement purpose. This is the common cause of actually evolving, fatigable weakness and preferentially affects ocular, facial and bulbar muscles. It is caused due to breaking down the communication between nerves and your skeletal muscles.
There is no cure for Myasthenia Gravis, but treatment can help to relieve sign and symptoms. Some of the myasthenia gravis symptoms are a weakness of arm or leg muscles, double vision, drooping eyelids, difficulty with speech, chewing, swallowing and breathing. It can affect the people of any age, but its more common in the women younger than 40 and in men older than 60.
Pathophysiology
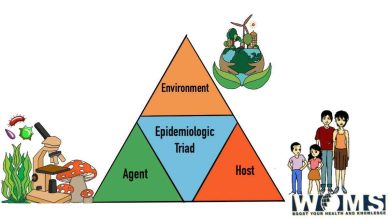
Myasthenia gravis is an autoimmune disease, most commonly (80% of cases) caused by antibodies to acetylcholine receptors in the past-junctional membrane of the neuromuscular transmission and complement-mediated inflammatory response reduces the number of acetylcholine receptors and damages the end plate. Other antibodies can produce a similar clinical picture, most notable autoantibodies to muscle-specific kinase (MuSK), which is involved in the regulation and maintenance of acetylcholine receptors.
About 15% of patients (mainly those with late-onset) have a thymoma, most of the remainder displaying thymic follicular hyperplasia. Myasthenic patients are more likely to have associated organ-specific autoimmune disease. Triggers are not always evident but some drugs (e.g penicillamine) can precipitate an antibody-mediated myasthenic syndrome that may persist after drug withdrawal. Other drugs, especially aminoglycosides and quinolones, may exacerbate the neuromuscular blockade and should be avoided in the patients with myasthenia.
Source: Davidson
Myasthenia gravis symptoms
Myasthenia gravis usually presents between the ages of 15 and 60 years and there is female preponderance in younger patients. In older patients, males are commonly affected. It tends to run a relapsing and remitting course.
The most evident symptom is fatigable muscle weakness; movement is initially strong but rapidly weakens as muscle use continues. The first symptoms are usually intermittent ptosis or diplopia. Some other symptoms of MG are:
- Difficulty in speech
- Problems with walking, lifting
- Facial paralysis
- Difficulty breathing
- Fatigue
- Hoarse voice
- Dropping of eyelid
- Double vision
There are no sensory signs of involvement of CNS, although the weakness of the oculomotor muscles may mimic a central eye moment disorder. Ventilator support may require when there is severe weakness of the respiratory muscles.
Is myasthenia gravis autoimmune?
Yes, myasthenia gravis is a chronic autoimmune neuromuscular disease that causes weakness in the skeletal muscle, which is responsible for the different body function such as breathing and movement of legs and arm.
Investigations
Intravenous injection of the shorter-acting anticholinesterase edrophonium bromide ( The tension test) is less widely used than before. Improvement in muscle function occurs within 30 seconds and usually persist for 2-3 minutes but the test is not entirely specific or sensitive. Cover with intravenous atropine is necessary to avoid bradycardia. Planning assessment beforehand (eg. Speech or limb movement) allows some objectivity in gauging the effect.
Repetitive stimulation during nerve conduction studies may show a characteristic decremental response. If the muscle has been clinically affected. Anti-MuSk antibodies are more common in acetylcholine receptors antibody-negative patients with prominent bulbar involvement. All patients should have a thoracic CT to exclude Thyoma, especially those without ant-acetylcholine receptor antibodies. Screening for associated autoimmune disorders, particularly thyroid disease, is important.
Management
The goals of treatment are to maximize the activity of acetylcholine at remaining receptors in the neuromuscular junctions and to limit or abolish the immunological attack on motor end plates.
The duration of action of acetylcholine is prolonged by inhibiting acetylcholinesterase. The most commonly used anticholinesterase drug is pyridostigmine. Muscarinic side-effects, including diarrhea and colic, may be controlled by propantheline. Overdosage of anticholinesterase drugs may cause a ‘cholinergic crisis’ due to depolarization block of motor end plates, with muscle fasciculation, paralysis, pallor, sweating, excessive salivation, and small pupils. This may be distinguished from severe weakness due to exacerbation of Myasthenia (‘myasthenia crisis’) by the clinical features and, if necessary, by the injection of a small dose of edrophonium.
Immunological treatment of myasthenia is given below. Thymectomy may improve overall prognosis but as]waits for clinical trial confirmation. Prognosis is variable and remissions may occur spontaneously. When myasthenia is entirely ocular, the prognosis is excellent and disability slight. Young female patients with generalized disease may benefit from thymectomy, while older patients are less likely to have a remission despite treatment. Rapid progression of the disease more than 5 years after onset is uncommon.
Immunological treatment of Myasthenia
Acute treatments
Intravenous immunoglobulin
- Lower production of antibodies and rapidly reduces weakness
- Plasma exchange
- Removing antibody from the blood may produce marked refinement; this is usually brief, so is normally reserved for myasthenic crisis or for pre-operative preparation
Long-term treatment
Glucocorticoid treatment
- Improvement is commonly preceded by marked exacerbation of myasthenia gravis symptoms, so treatment should be initiated in the hospital
- Usually necessary to continue treatment for months or years, risking adverse effects
Pharmacological immunosuppression treatment
- zathioprine 2.5mg/kg daily reduces the necessary dosage of glucocorticoids and may allow their withdrawal. Effect on clinical features may be delayed for months
- Mycophenolate mofetil; less commonly used
Thymectomy
- Should be considered in any antibody-positive patient under 45 years with myasthenia gravis symptoms not confined to extraocular muscles, unless the disease has been established for more than 7 years
- Likely to be required for thymoma
Check out this article which is similar to this disease – Guillain-Barre syndrome (GBS)
Summary
Myasthenia gravis affects 50 to 200 per million people in the world. It is newly diagnosed with three to 30 million people per year. Diagnosis is becoming easier due to more awareness programme. It commonly occurs in women of age 40 and men of age 60. It is uncommon in children. With the treatment of most of the effect, people tend to have a normal life and also a normal life expectancy.